Global health agencies have recently issued more alerts about medication safety, especially drugs that may affect the heart and blood vessels. These updates are part of routine surveillance, where regulators may order temporary withdrawals, label changes, or stronger warnings. As the article notes, such actions “do not necessarily mean a medication is universally dangerous” but reflect new scientific information meant to keep patients safe.
Several categories of medicines have faced review, including hormonal contraceptives, some anti-inflammatory drugs, certain weight-loss products, and a few COVID-19 treatments. Concerns often involve cardiovascular risks like “blood clots, embolisms, strokes, or heart attacks.” Agencies such as the FDA and EMA remind the public to stay informed and report side effects so authorities can respond quickly.
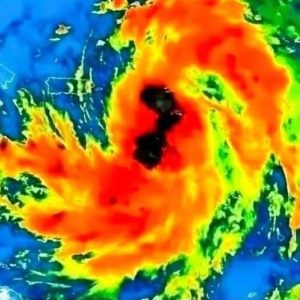
Many of these issues center on thrombi—“commonly known as blood clots.” While clotting helps stop bleeding, trouble begins when clots form unnecessarily and block blood flow. Deep vein thrombosis may cause swelling or pain, and if a clot travels to the lungs, it can lead to a pulmonary embolism. Arterial clots can trigger a heart attack or stroke, both medical emergencies.
Some medications may influence clot risk, but this varies widely. For example, hormonal contraceptives carry a small, well-known risk, and doctors consider factors like age, smoking, and medical history before prescribing. NSAIDs, high doses, unregulated supplements, or improper use can also increase danger.
Health agencies urge people to avoid panic, ignore misinformation, and practice “informed caution.” Patients should understand their medications, watch for symptoms, and never stop treatment without medical advice.